Nourishing Hope: The Vital Role of Nutrition and Diet in Managing IBD Flare and Remission
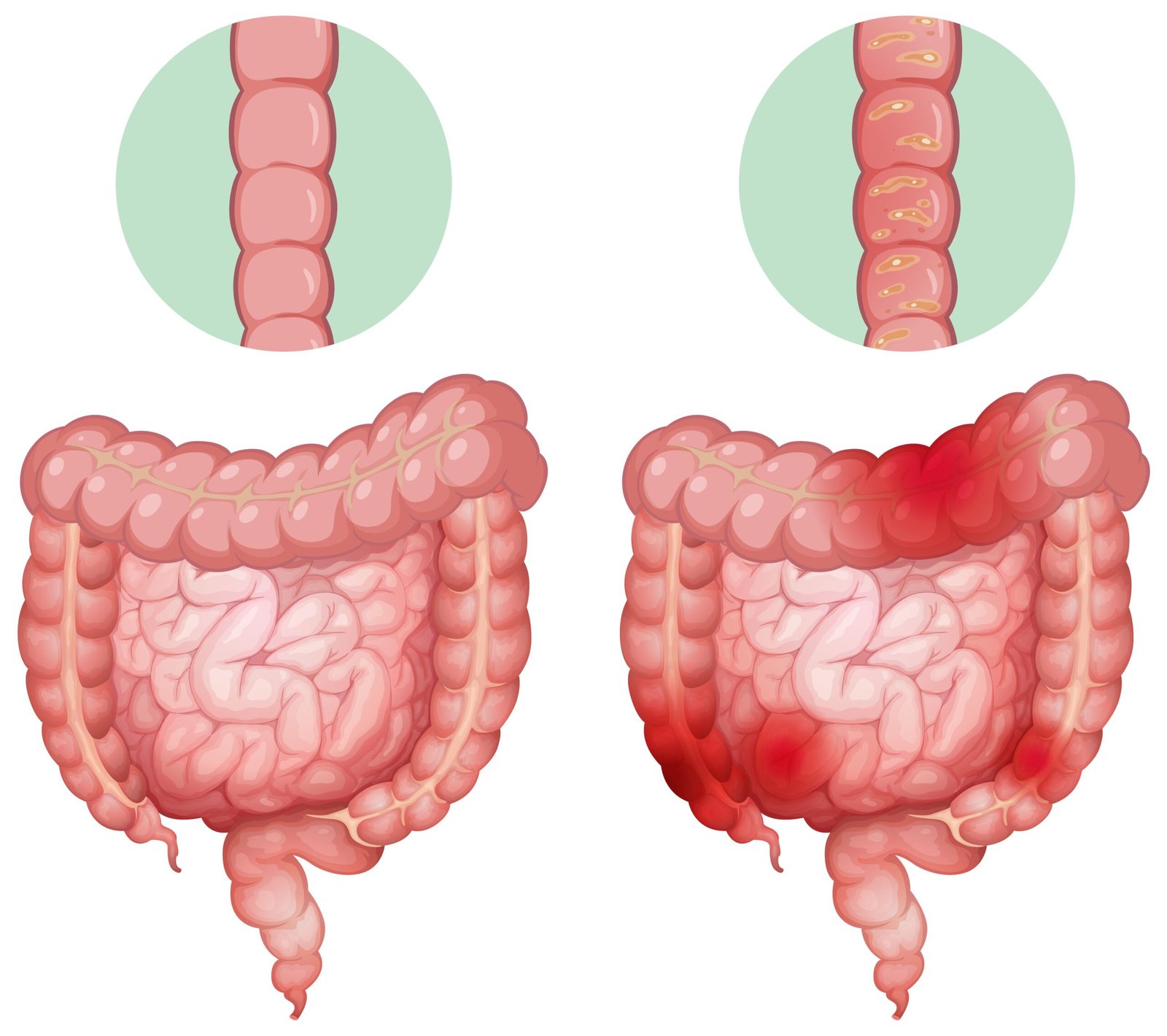
Inflammatory Bowel Disease (IBD) is a chronic condition that affects millions of individuals worldwide. The two primary forms of IBD, Crohn’s disease and ulcerative colitis, can lead to debilitating symptoms, including severe abdominal pain, diarrhea, and nutritional deficiencies. While medical treatments are essential, the role of nutrition and diet in managing IBD during both flare and remission phases cannot be underestimated.
Understanding IBD
IBD is characterized by chronic inflammation of the gastrointestinal tract. During a flare-up, the inflammation becomes more severe, causing symptoms to worsen. However, during remission, the inflammation subsides, and patients may experience milder or no symptoms at all. Managing both phases effectively is vital for patients’ overall well-being and quality of life.
Nutrition During Flare-Ups
During an IBD flare-up, the inflamed intestinal lining is particularly vulnerable. Proper nutrition plays a pivotal role in providing relief and aiding recovery.
Low-Residue Diet: A low-residue diet is often recommended during flare-ups. This diet minimizes fiber intake, reducing the bulk and frequency of bowel movements, which can alleviate abdominal discomfort.
Avoid Trigger Foods: Identifying and avoiding trigger foods is essential. These foods can vary from person to person but commonly include dairy products, spicy foods, and high-fat items.
Nutritional Supplements: Malnutrition is common in IBD patients, especially during flare-ups. Nutritional supplements may be prescribed to address deficiencies and provide essential nutrients.
Hydration: Maintaining adequate hydration is critical to prevent dehydration due to diarrhea. Water, herbal teas, and electrolyte-rich beverages can help.
Nutrition During Remission
The goal during remission is to maintain gut health, prevent relapses, and improve overall well-being.
Balanced Diet: Emphasize a balanced diet rich in fruits, vegetables, lean proteins, and whole grains. These foods provide essential nutrients and promote gut health.
Probiotics: Incorporating probiotic-rich foods like yogurt or fermented foods can help maintain a healthy gut microbiome, potentially reducing the risk of relapse.
Omega-3 Fatty Acids: Foods like fatty fish, flaxseeds, and walnuts provide omega-3 fatty acids, which have anti-inflammatory properties and may help prevent flare-ups.
Fiber Gradual Introduction: If tolerated, gradually reintroduce high-fiber foods to maintain regular bowel movements and promote colon health. Fiber can help prevent constipation and diverticulosis.
Monitor Trigger Foods: Continue to monitor individual trigger foods and avoid them to minimize the risk of symptom recurrence.
Professional Guidance and Individualization
It’s crucial to note that IBD is a highly individualized condition, and what works for one person may not work for another. Consulting with us is essential. We can provide personalized dietary recommendations, monitor nutritional status, and adjust the diet plan based on your unique needs and disease activity.
Conclusion
Nutrition and diet play a vital role in the management of IBD, both during flare-ups and remission. A well-balanced diet tailored to the individual’s needs can help alleviate symptoms, promote healing, and reduce the risk of relapse. It’s important for individuals with IBD to work closely with healthcare professionals to develop a dietary plan that suits their specific condition and goals. By embracing the power of nutrition, individuals with IBD can nourish hope for a healthier future.
References:
Torres, J., et al. (2017). Ulcerative colitis as a progressive disease: The forgotten evidence. Inflammatory Bowel Diseases, 23(1), 27-34.
Ananthakrishnan, A. N. (2015). Nutrition and inflammatory bowel disease: An update. Current Opinion in Gastroenterology, 31(5), 340-346.
Levine, A., et al. (2011). ESPGHAN revised porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. Journal of Pediatric Gastroenterology and Nutrition, 53(6), 795-796.
Ng, S. C., et al. (2017). Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based studies. The Lancet, 390(10114), 2769-2778.
Hou, J. K., et al. (2014). Dietary intake and risk of developing inflammatory bowel disease: A systematic review of the literature. The American Journal of Gastroenterology, 109(11), 1738-1747.
Gibson, P. R., & Shepherd, S. J. (2005). Evidence-based dietary management of functional gastrointestinal symptoms: The FODMAP approach. Journal of Gastroenterology and Hepatology, 25(2), 252-258.